Background:
Major adverse cardiovascular events and all-cause mortality are higher and well-known complications of COVID 19 infection in cancer patients. However, considering limited data comparing the trends and outcomes in COVID-19 patients with and without multiple myeloma (MM), this population-based study evaluates the epidemiological trends and characteristics of sex, race, and co-morbidities to further understand the outcomes in COVID-19 patients hospitalized with or without Multiple Myeloma (MM).
Methods:
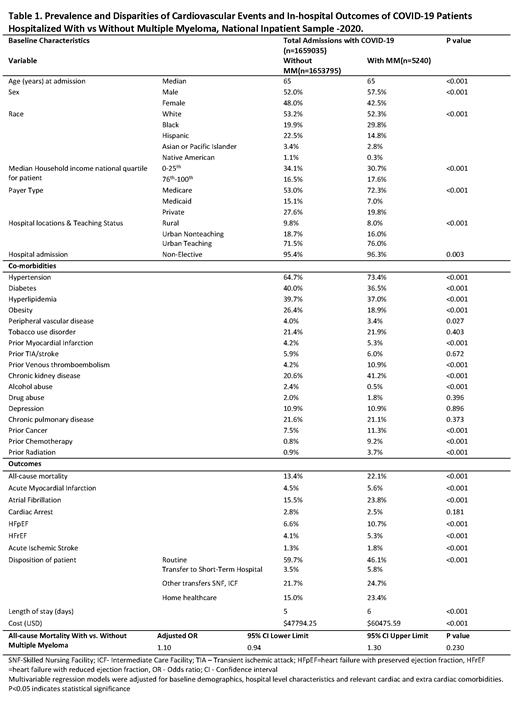
The US National Inpatient Sample for 2020 was assessed in hospitalized patients using relevant ICD-10 CM diagnostic codes and a retrospective cohort study was conducted. The cohort consisted of COVID19 patients which were then divided into two categories based on the occurrence of MM. The impact of COVID19 in the prevalence and outcomes of cardiovascular events in patients with and without MM was evaluated using multivariable regression analysis to assess the independent predictors of all-cause mortality.
Results:
We identified 1,659,035 COVID-19-related admissions, of which, 5240 (0.3%) patients had MM and 1,653,795 without MM. A median age was found to be 65 years in both the cohorts. Cohort with MM often consisted of male (57.5% vs. 52%), black (29.8% vs. 19.9%), Medicare enrollee (72.3% vs. 53%), admissions at urban teaching hospital (76% vs. 71.5%), non-electively admitted patients (96.3% vs 95.4%) compared to cohort without MM. Hypertension (73.4% vs 64.7%), prior MI (5.3% vs. 4.2 %), prior Venous thromboembolism (10.9% vs. 4.2%), CKD (41.2% vs. 20.6%), prior cancer (11.3% vs. 7.5%), prior chemotherapy (9.2% vs. 0.8%), prior radiation (3.7% vs. 0.9%), Higher length of stay (6 vs. 5 days); higher cost ($60475.59 vs. $47794.25) were also noted more frequently in MM cohort with significant p-value of <0.05. Whereas the cohort without MM consisted of higher proportion of females (48% vs. 42.5%), white (53.2% vs. 52.3%), Hispanics (22.5% vs. 14.8%), Asian or Pacific islanders (3.4% vs. 2.8%), Native Americans (1.1% vs. 0.3%), patients from lower household income (34.1% vs. 30.7%), Medicaid enrollees (15.1% vs. 7.0%), and patients with diabetes (40% vs. 36.5%), hyperlipidemia (39.7% vs. 37%), obesity (26.4% vs. 18.9%), peripheral vascular disease (4% vs. 3.4%), alcohol abuse (2.4% vs. 0.5%). MM patients were at increased risk of death during COVID19 hospitalizations, with equal risk amongst Male (22.2%) and Female (22.0%), compared to those without MM (p < 0.001). MM patients of Hispanic race were at increased risk of mortality during COVID-19 hospitalization (30.1%) (p<0.001). Additionally, MM patients of both sexes were at increased risk of mortality during COVID-19 hospitalizations given history of atrial fibrillation, with increased risk in Male patients (26.7 %) compared to Female patients (19.8 %) (p <0.001). Amongst different races, MM patients with atrial fibrillation of Hispanic race had increased mortality on COVID-19 hospitalizations (17.1%) compared to non-MM Hispanic patients (7.7%) (p <0.001). The MM group exhibited higher percentages of all-cause mortality (22.1% vs. 13.4%), acute myocardial infarction (5.6% vs. 4.5 %), atrial fibrillation (23.8% vs. 15.5%), heart failure with preserved ejection fraction (10.7% vs. 6.6%), heart failure with reduced ejection fraction (5.3% vs. 4.1%), and acute ischemic stroke (1.8% vs. 1.3%) without any significant difference for cardiac arrest. However, on multivariable regression analysis adjusted for covariates, there was no difference between all-cause mortality in COVID19 patients with MM vs. without MM (p = 0.230).
Conclusions:
Multiple Myeloma in COVID19 is associated with higher cardiovascular events and death during hospitalization, however, the study failed to show a statistically significant difference when adjusted for potential confounders. Prevailing sex and race-based disparities in cardiovascular outcomes in COVID19 patients with MM warrant future longitudinal studies.
Clinical Implications:
Clinicians can use this data to identify MM patients with COVID-19 to implement appropriate management strategies to reduce the adverse outcomes. Given the long-term complications and progression of MM, it remains crucial to understand the relationship and systemic effects of COVID-19 on patients with MM and impact of different risk factors and co-morbidities on long-term outcomes in post-COVID phase.
Disclosures
No relevant conflicts of interest to declare.